
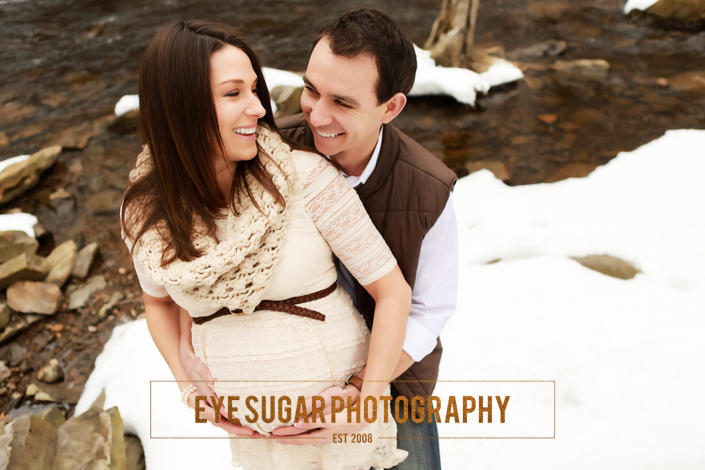
It was my second ultrasound of the day; one that brought a different kind of anticipation. The first ultrasound was one of the most incredible experiences of my life, at 19 weeks pregnant my husband and I found out that we were having a baby boy. I couldn’t shake my permanent smile as I walked in for the second ultrasound; an appointment that I assumed would be a quick check of a thyroid nodule to confirm it was benign. But a week later the findings didn’t echo the sentiment of my first ultrasound, I was diagnosed with papillary thyroid cancer.
It all started with an “annual” physical with my general physician (GP); annual in quotes because I hadn’t gone to see an actual GP for a physical since my college days. I was healthy, athletic, and felt great. I saw my ob/gyn annually, so why tack on another appointment to my busy schedule simply to hear that all was well? But after becoming pregnant with my first child, I became extremely ill with food poisoning and my OB practice strongly suggested that I get a GP.
My physical started out exactly as I had anticipated, fit and healthy, until my GP checked my throat area. “Did you know you have a lump on your thyroid?” I didn’t even know what my thyroid was, let alone that there was something unusual with it. My GP arranged an ultrasound a few days later, which showed a large (1.6cm) nodule with micro-calcification and blood flow as well as multiple other smaller nodules. Despite having no family history and no history of exposure to radiation, the research I’d done told me these were all indicators of cancer. While they said it was probably fine, after all, 90% of thyroid nodules are harmless and non-cancerous, it prompted a follow-up fine-needle aspiration biopsy on the large nodule. A day after the biopsy I was diagnosed with papillary thyroid carcinoma. My reality was that I was 20 weeks pregnant with the “C” word. It definitely was not part of what I had pictured or planned to navigate during my first pregnancy. Here are things that helped me through the past few months post-diagnosis.
Research: In the days after my biopsy, before my diagnosis, I was a complete Google sponge on everything about thyroid nodules and thyroid cancer, so when I was diagnosed with papillary carcinoma, I knew that I was lucky. I had the “best” cancer anyone could be diagnosed with, if there is such a thing. It tends to be minimally invasive and slow growing. There are several types of thyroid cancer and the survival rate for those with papillary (which is the most common type) is at least 95%, and in my case due to age and gender, closer to 100% with appropriate treatments.
In doing my pre-diagnosis research, I was on the fence about whether I would want to have surgery before or after delivery, and wanted to have both options on the table. Christmas was a month away and from my research I found that thyroid surgery while pregnant ideally takes place in the 2nd trimester. That left me with 7 weeks to have surgery if I chose to do it pre-delivery. Knowing this timeline, I researched and called three major-area hospitals pre-diagnosis to talk to their endocrinology surgery department about timing, insurance coverage, and approach if I were diagnosed with cancer. When I got the call with the diagnosis, I was already prepared to make the call to my selected hospital for my first appointment with the endocrine surgeon.
Preparation: I was able to get in for my first appointment with an endocrine surgeon a couple weeks later. After doing a lot more research, I prepared a list of questions to ask the surgeon and brought my family along for support. Right off the bat the surgeon put me at ease. Thyroidectomies are her bread & butter. She does multiple thyroidectomies a week and found my scenario to be fairly routine. She was confident that I would make a full recovery after surgery. Coming prepared with questions was extremely helpful so that I knew all my concerns were addressed. My biggest concerns were timing of surgery due to pregnancy, ability to test lymph nodes for spreading while I’m in surgery, risk of vocal cord paralysis, and if/when I would need to take the Radioactive Iodine, RAI, pill. (I’ve shared my list of questions at the end.)
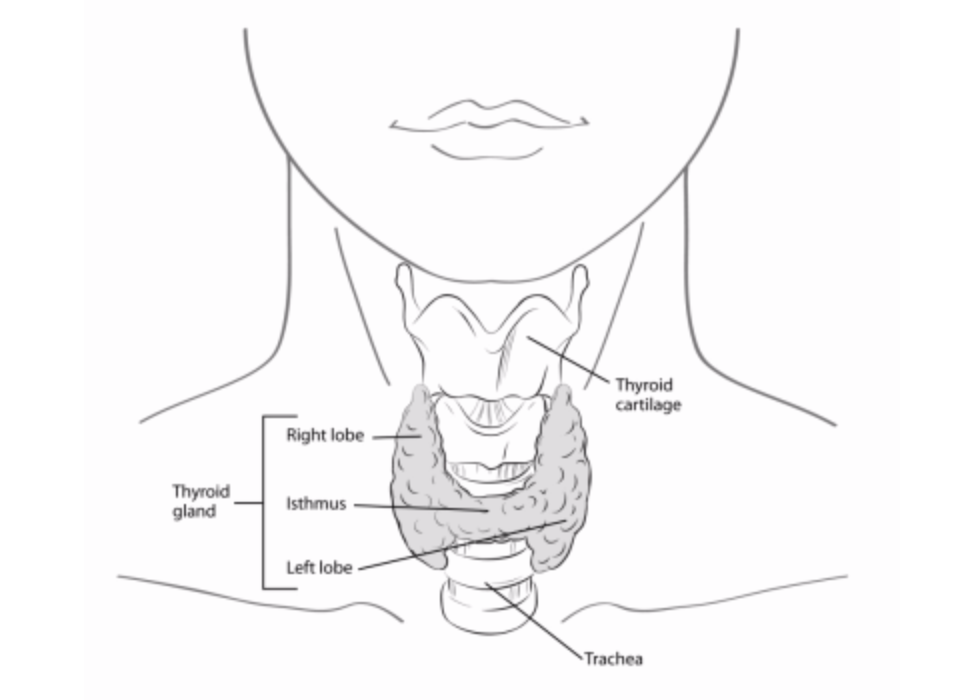
I learned that in my circumstance, due to location of my nodule (on the isthmus) and due to the size of my nodule, a thyroidectomy (complete removal of the thyroid) would be recommended. The choice was ultimately mine on whether to have surgery before or after the baby arrives, however the doctor said her recommendation was to wait until 4-8 weeks after baby is born to have surgery. This was based on the risk of complications in pregnancy during surgery being greater than the risk of living with slow-growing papillary carcinoma for the next 6 months. She confirmed that during surgery they could immediately test suspicious lymph nodes and if they were of concern, remove them at that time. This was a big deal because I didn’t want to have a second surgery for lymph nodes (in my research I learned that some hospitals are unable to test while you’re in surgery). She also assured me that my parathyroid glands would be preserved and that they would continuously test and monitor my laryngeal nerves during surgery. Her comfort level in this was a big deal, the risk of losing my voice and not being able to talk to my baby (and everyone else in my life) is a scary one!
The RAI pill was a concern of mine because it will force me to stop breastfeeding. I learned that the recommendation on the RAI pill will come post-surgery, partly depending on if the cancer appears to have spread to lymph nodes and/or is multi-focus (more than one cancerous nodule). If I have to take the RAI pill, then my doctor supports my wish to breastfeed for a period of time after surgery, and noted that I need to wait at least 2 months after I stop breastfeeding before I can take the RAI pill. The RAI pill, if I need it, will require me to be isolated from adults for a period of time and from babies/children for a longer period of time as I will be radioactive (from what I understand it’s somewhere between 4-10 days). Taking this pill will also delay our trying for a second child for 6mo to 1yr to avoid risk to the fetus. Ideally I won’t have to take this pill (fingers crossed), but time will tell.
The last piece of the puzzle after surgery is getting into balance with a new thyroid hormone replacement pill I’ll have to take daily for the rest of my life. This is something I’ll spend more time figuring out post-surgery with my endocrinologist. From what I’ve read and heard from friends, this is a journey of its own.
Support: The best thing in the world for me was to know that I wasn’t alone. It’s the main reason I wanted to write about my experience. Being able to hear and read about other peoples experiences with thyroid cancer both when pregnant and not, was so helpful. I went from not knowing what a thyroid is to finding out how many people I am connected to have thyroid issues, ranging from cancer, to hormone imbalances, to Hashimoto’s. Thyroid issues affect a lot more people that I ever realized. I’ve spent hours getting advice and support from friends and family in person, on the phone, via email, and even good old snail mail. It has warmed my heart and made this journey through pregnancy and cancer so much easier.
What I’ve learned from all of this so far is that an annual physical is important no matter how healthy you feel, to be your own advocate in getting answers to all of your questions, and not to be afraid to reach out to others, the best advice and support has come from friends and family both far and near.
My surgery is now scheduled for 8 weeks after my due date and honestly it’s the last thing on my mind. Having done the research, getting all my questions answered by the surgeon, and having the most supportive friends and family, has made any cancer worries all but disappear. I truly have been able to focus on the joys of being pregnant and the anticipation of all the wonderful life changes this little boy will bring to our lives.
Laura is due with her first baby on April 22, 2015.
References:
http://www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf
http://www.nlm.nih.gov/medlineplus/ency/article/000331.htm
http://press.endocrine.org/doi/full/10.1210/jc.2010-1624
My list of questions for the surgeon:
- Is the recommendation to do a total thyroidectomy?
- What is the recommendation for timing of surgery? Possible risks of surgery before the baby is born? Proper thyroid hormone replacement ratios to support me and baby?
- If I’m waiting to do surgery until after the baby is born, how will we continue to monitor the growth of the tumor until surgery? What changes would we expect for the tumor throughout the rest of the pregnancy and breast feeding?
- Are my current hormone levels normal? How does this effect development of the baby?
- What are the risks for the cancer spreading based on what is seen on my biopsy/ultrasounds?
- How is the approach different for a nodule located on the Isthmus? Will I need a thyroidectomy plus a central compartment neck dissection?
- How will you know if the cancer has spread to lymph nodes or other areas? Do I have enlarged lymph nodes? Do you test/remove lymph nodes while I’m in surgery?
- What is the risk of injury to the parathyroid glands and recurrent laryngeal nerves? Will the parathyroid glands be preserved? Risk of transient or permanent vocal cord paralysis?
- Will I need the Radioactive Iodine (RAI) pill? My concerns include Breast feeding and desire to have a second child.













this same exact thing happened to me when I was pregnant with my second child. The same day they told me I was pregnant they also palpated the nodule on my thyroid. I, too, waited till after the baby was born to have my thyroidectomy. I’m six years postop. All of my checkups have been very good. My baby is 6 years old and perfect too.
Love & prayers and many blessings for your little guys arrival. Being a boy mama is amazing!!!! 🙂
The same thing happened to my twin sister 2 years ago when she was pregnant. She had her thyroid removed when she was around 10 weeks pregnant. We live in Houston and she is fortunate enough to see a thyroid specialist at MD Anderson. Her doctor recommended not doing the radioactive iodine. There is some new research that doing the radioactive therapy is not always the best option. I reccomend checking it out. The good news is that thyroid cancer has a great prognosis. I went and got checked and had non-cancerous thyroid growths removed. I reccomend all ladies asking their obgyn to scan their neck the next time they have an appointment. Most insurance companies will cover it. Both my twin and my blood thyroid levels always came back normal. You have to get the neck scan to be more accurate.
From a fellow mom and an oncology RN who has much experience administering and monitoring those under RAI treatment, you are one impressive patient! Way to go — and very best wishes in this next chapter. Sounds like you’ll rock it. 🙂
[…] Check out her blog at Madison City Moms Blog. […]
I was diagnosed with papillary thyroid cancer 3 years ago! I had no children at the time, but knew I wanted them in the future. After my total thyroidectomy, I opted not to go through with the RAI, my gut instinct told me not to and while my endocrinologist suggested I do it, she supported my decision not to. I was pregnant a few months later (which definitely would not have been possible had I been “radioactive”) My checkups have all been perfect and at my most recent appointment my endo actually told me that the guidelines for RAI have changed and she is very grateful that I didn’t go through with it!
I’m dealing with this now… papillary thyroid cancer one nodule on left lobe… I don’t want rai if I have a say… how does this conversation even go? My right lobe was already removed 2 years ago and it has completely grown back which I say I a miracle considering I have cancer now on the opposite lobe but my dr thinks it’s weirs since the thyroid doesn’t do this… I would like to keep my right lobe if I can… was it hard to get the dr on board with no rai? Or a fight? Was only taking one lobe an option ever?